The shooting of a man with Traumatic Brain Injury (TBI) by police in Charlotte NC made me think about veteran families who live with TBI. Mr. Scott, the man in Charlotte NC, had suffered TBI from a motorcycle accident and some believe his TBI may have played a part in his death. So many folks with TBI suffer from impulse control issues, which means that they make very bad decisions. Mr. Scott was not a veteran, but I began to think of how easily he could have been a veteran. The discussion about TBI due to its prevalence in the veteran community is needed. I know many veterans who suffer from TBI and I see how it affects them, their families and their lives, it’s not easy being married to someone with TBI, often it is like being married to a teenager.
There are many causes of TBI or mTBI in the military. Accidents resulting in head trauma, being knocked unconscious by explosions or improvised explosive devices (IED’s), shrapnel wounds or bullet wounds are common. According to the Veterans Administration (VA) an estimated 22% of all combat casualties from Operation Iraqi Freedom (OIF), Operation Enduring Freedom (OEF) and Operation New Dawn (OND) have brain injuries. The Department of Defense (DOD) puts the number of TBI victims at 50,000, and the Pentagon at 115,000. However, non-military connected entities such as the Brain Injury Association of America (BIAA) places the number of veterans with TBI at 360,000 and the RAND corporation suggests as many as 400,000 veterans suffer with TBI. To say the least, it is unsettling to see the difference between the DOD’s numbers and the BIAA numbers. These numbers do not include those veterans who struggle with this problem but never report their difficulties so that they could be diagnosed and treated. The VA also estimates that 12% of Vietnam Veterans suffer from TBI but there are no hard numbers for them because TBI was not tracked.
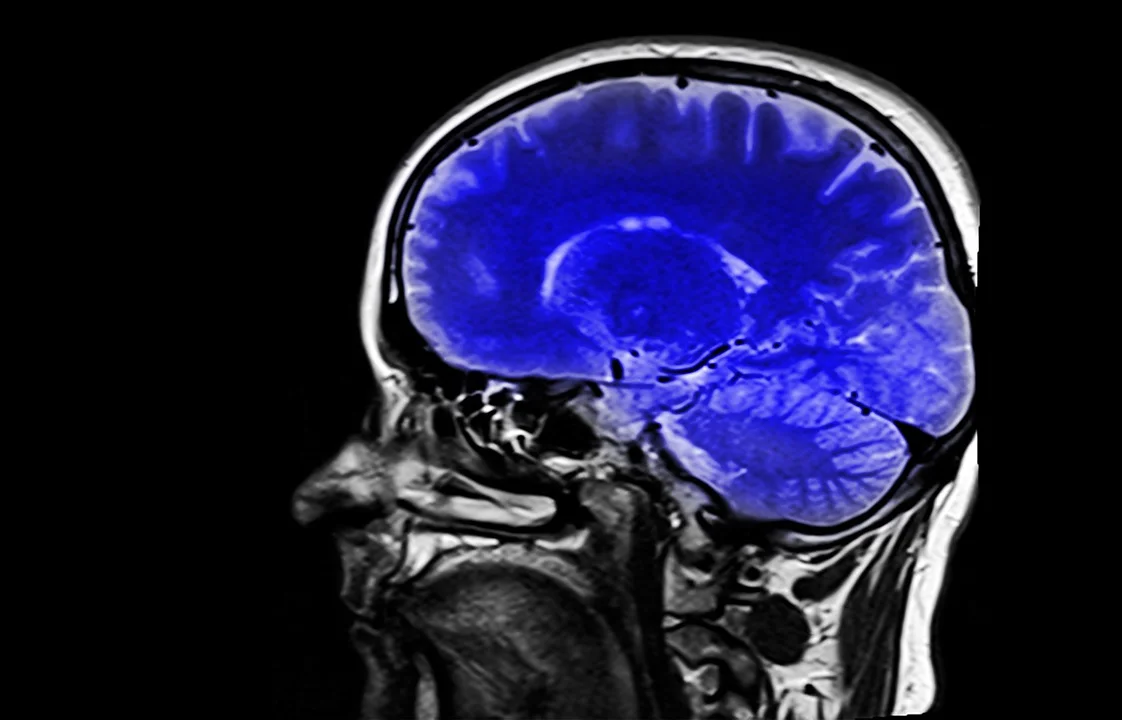
The definition of TBI is a non-degenerative, non-congenital insult to the brain from an external mechanical force, possibly leading to permanent or temporary impairment of cognitive, physical, and psychosocial functions, with an associated diminished or altered state of consciousness. If the incident causes loss of and /or confusion and disorientation longer than 30 minutes TBI is likely. It is unknown how TBI interferes with the brain and is often confused with Post Traumatic Stress Disorder PTSD because the signs often overlap. TBI can be difficult to diagnose, recognize or treat. Severe TBI can leave a person unable to function normally.
Mild Traumatic Brain Injury (mTBI) is known as a concussion. mTBI can be considered if the loss of consciousness, confusion, or disorientation from the event is less than 30 minutes. We have been hearing about mTBI in the media because of the National Football League (NFL) but not veterans who face mTBI from concussions. Assessments such as a MRI’s or CAT scans can look normal and mTBI still exist. Residual symptoms for mTBI can be seen for 18-24 months after the incident. Each mTBI event increases the chances of permanent brain damage.
Discussing “brain damage” is scary for family members. The recovery of a brain injury is unlike other seen or internal injuries. TBI or mTBI can change an individual’s personality causing the individual to act differently than they did before their injury. Frequently family members are the first to see the changes and do not know what they are seeing, all they see is an irrational loved one. TBI or mTBI symptoms may not be seen right away, without professional help a family member might not know their loved one is suffering from either. Some TBI and mTBI veterans have co-morbid problems with PTSD, chronic pain, and substance abuse among the most common symptoms masking the brain damage. These medical issues can complicate treatment and limit the ability to successfully find a single diagnosis for TBI or mTBI. Even well trained professionals struggle diagnosing TBI and mTBI at times because the co-occurring issues disguise the real issue.
Veterans act differently in theatre than at home, only family members know what the veteran was like before they left. If the veteran spent an extended period of time in the hospital with no visible wounds or were un- conscious for longer than 30 minutes, there is a chance the veteran has TBI. On the other hand, many veterans will not admit to being “out” if the duration was short making mTBI harder to diagnose. mTBI is not mild to families who live with it and can be devastating to the family unit. Families should understand the nature of veteran’s head injuries can be different for each individual and produce diverse experiences.
I can only imagine how the events in Charlotte N.C. impacted veteran’s spouses who live with TBI or mTBI veteran. Mr. Scott could have been any one of our veterans. Family members understand what it is like to live with someone with brain damage, police don’t. Hopefully the incident in Charlotte N.C. will bring attention to TBI and cause better training for police not only for TBI but all mental health issues police officers face. It is also important for veteran’s families and veterans themselves understand that in many cases with hard work, appropriate treatment, and healthy behaviors, their veteran’s issues can likely improve.
Common TBI signs: Understand TBI and mTBI signs can overlap
Lack of Attention
Lack of Concentration
Distractibility
Memory issues
Speed of Processing
Confusion
Perseveration
Impulsiveness
Language Processing
“Executive functions” (Decision Making Ability)
Speech, Language and writing difficulties
Chronic pain
Sleep disorders
Menstrual difficulties
Irritability
Aggression
Depression
Denial/lack of awareness
Common Symptoms of TBI
Fatigue
Headaches
Visual disturbances
Memory loss
Poor attention/concentration
Sleep disturbances
Dizziness/loss of balance
Irritability-emotional disturbances
Feelings of depression
Overlapping symptoms between PTSD and TBI
Depression
Anxiety
Irritability
Anger
Trouble Concentrating
Fatigue
Hyperarousal
Avoidance
Learn more how to save veteran's life. CLICK HERE to get your FREE Training.
For questions or comments, I can be reached at afterdutyvets@gmail.com or visit our website at marriedtoptsdpro.com and like us on Facebook at Married to PTSD Pro.